Federal Appeals Court Strikes Down Graphic Smoking Warnings
Posted on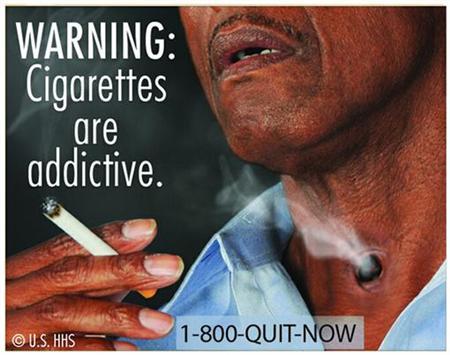
Undoubtedly this smoking flap will be headed to the United States Supreme Court.
A US court on Friday shot down orders to slap graphic anti-tobacco messages on cigarette packs, saying the government overstepped its authority by trying to “browbeat” smokers into quitting.
In line with campaigns in several other nations, the United States planned from September 22 to require images on cigarette packs including a man smoking through a hole in his throat and a body with chest staples on an autopsy table.
In a 2-1 decision, the US Court of Appeals in Washington said that the images planned on cigarette packs were not necessarily false but they went beyond “pure attempts to convey information to consumers.”
“They are unabashed attempts to evoke emotion (and perhaps embarrassment) and browbeat consumers into quitting,” Judge Janice Rogers Brown, who was appointed by former president George W. Bush, wrote for the majority.
She also said that the US Food and Drug Administration “has not provided a shred of evidence” that graphic warnings directly reduced rates of smoking.
The graphic ads, as I have said before, don’t really bother me. I, also, don’t think anyone will be deterred from smoking because of them.
Hopefully, the entire flap will be moot as more and more Americans abandon the smoking habit/addiction.